Development of an Overdose Model
This research provides an accurate way to model overdose in the lab, using human brain cells programmed to respond to many different opioids. Amid an increasingly deadly opioid crisis, this tool can be used to screen medications to reverse overdoses from potent synthetic opioids like fentanyl.
Rebecca Baker. Ph.D.
Director of the Helping to End Addiction Long-term® Initiative, or the NIH HEAL Initiative® at the National Institutes of Health (NIH)
This system has implications for drug discovery and the development of more effective personalized medicines to combat the opioid crisis. It has potential as an alternative to animal models in determining effects of biological therapeutics, including pair modulations and alternatives to naloxone.
Danilo Tagle, Ph.D.
Director, Office of Special Initiatives
National Center for Advancing Translational Sciences (NCATS)
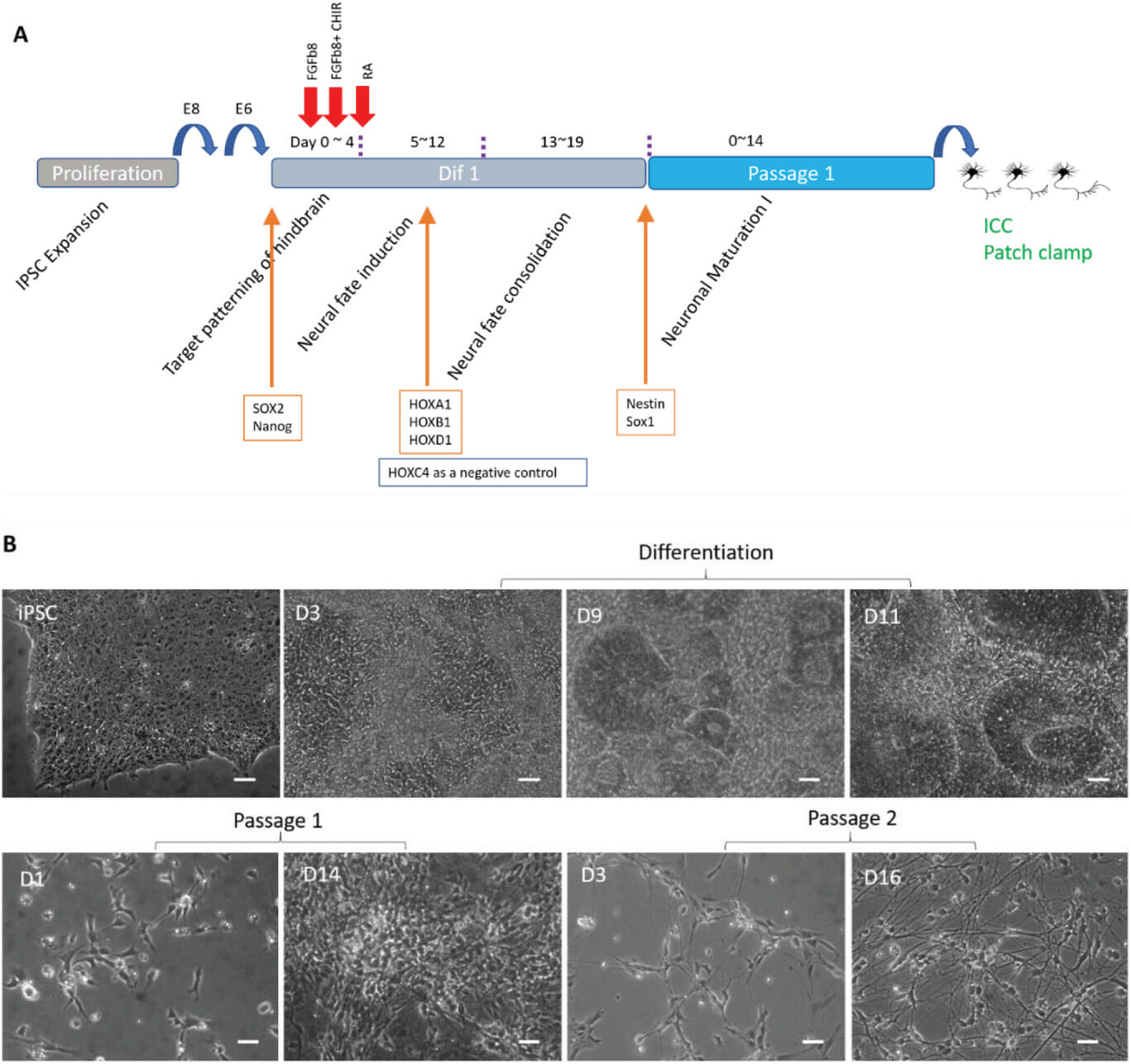
New Study describes first, functional human model to investigate Opiate Overdose and Recovery
FOR IMMEDIATE RELEASE: Orlando, Florida: A research team from the University of Central Florida and Hesperos, a pioneer in human-on-a-chip technology, has developed the first human model to study the effects of an opioid overdose and reversal with naloxone. The study, "Human IPSC-Derived PreBötC-like Neurons and Development of an Opiate Overdose and Recovery Model" (doi.org/10.1002/adbi.202300276) was published in Advanced Biology on September 7, 2023. The paper describes the development of human preBötC neurons from induced pluripotent cells (iPSCs) and the establishment of a human model that mimics opioid overdose with four opioids and the recovery of neuronal activity with naloxone treatment.
“I am incredibly proud of our team's groundbreaking work that will provide invaluable insights into understanding opioid addiction and recovery, paving the way for more effective treatments and ultimately saving lives. We hope this exciting first step will play a significant role in understanding and developing treatment solutions for this devastating crisis.”
- J Hickman, Professor UCF and Chief Scientist, Hesperos
The PreBötC brain region is responsible for automatic breathing regulation and is what shuts down first during an overdose (causing asphyxiation and ultimately death). The dose-dependent inhibition of these neurons’ activity was demonstrated with four opioids, including Fentanyl - the primary culprit of overdose deaths. Naloxone, the most widely used recovery medication, was used in each case to rescue activity, further replicating the response seen in patients.
Opioid overdose is the leading cause of drug lethality, posing an urgent need for investigation. Prior to this study, the best models available have been animal based which are known to have limited translation to humans. The development of this human model is a significant advancement in the field, bringing the medical community closer to finding a solution to this public health emergency.
“This research provides an accurate way to model overdose in the lab, using human brain cells programmed to respond to many different opioids,” said Rebecca Baker. Ph.D., Director of the Helping to End Addiction Long-term® Initiative, or the NIH HEAL Initiative®, at the National Institutes of Health (NIH). “Amid an increasingly deadly opioid crisis, this tool can be used to screen medications to reverse overdoses from potent synthetic opioids like fentanyl.”
This is the first step of the project that seeks to establish a five-organ, Human-on-a-Chip, including PreBötC neurons, liver, heart, kidney, and skeletal muscle, to monitor organ-specific, functional changes through each opiate-induced overdose and rescue to understand not only the effect of overdose but repeat application of naloxone for off-target toxicity of the non-neuronal organ constructs.
The project was funded by the National Center for Advancing Translational Sciences (NCATS) as part of NIH’s HEAL Initiative. Established in 2018, the HEAL Initiative is an aggressive effort to find scientific solutions that improve the understanding and treatment of opioid addiction.
“This system has implications for drug discovery and the development of more effective personalized medicines to combat the opioid crisis,” said Danilo Tagle, Ph.D., from NCATS. “It has potential as an alternative to animal models in determining effects of biological therapeutics, including pair modulations and alternatives to naloxone.”
Funding Support: NIH Grant 4UH3TR003081-02